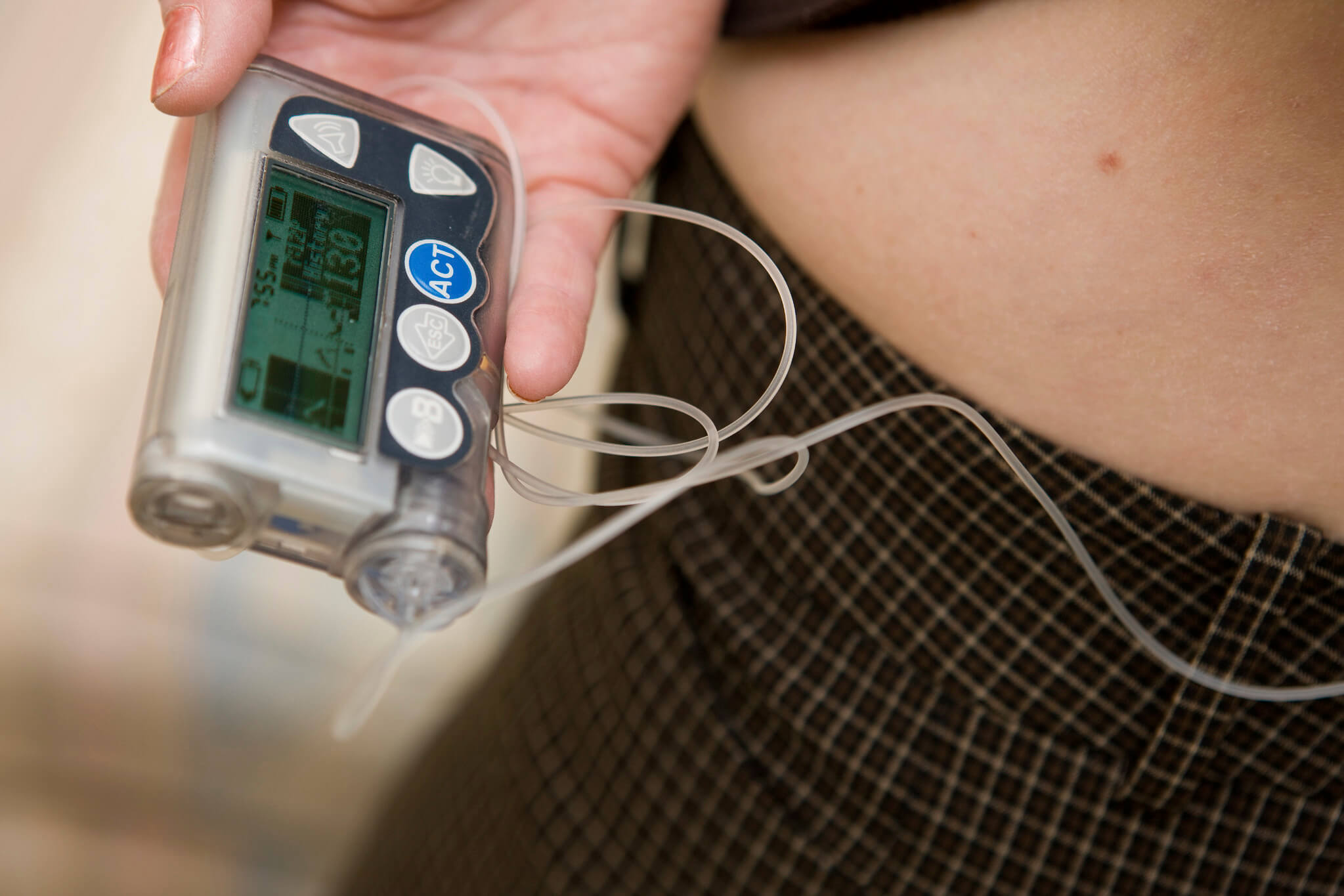
For individuals living with diabetes and relying on an insulin pump for their insulin delivery, the prospect of diving into the water during the sweltering summer heat brings along a wave of questions and concerns such as: “Will water damage my device?”, “How will my body respond?”, and, “Can I safely swim with my insulin pump on?”
In the following sections, we’ll dive deeper into the various aspects of swimming with an insulin pump, and answer the most common questions you might have.
Is it safe to swim with an insulin pump on?
Yes, you can swim with an insulin pump if it’s water-resistant or waterproof. But should you? Regardless of an insulin pump’s water resistance, it is generally not recommended to swim with one on because water exposure can potentially damage the device over time.
If you accidentally submerge an insulin pump in water, know that pumps that are waterproof or water-resistant can typically be submerged for 30 minutes at a depth of 1 m (3 ft). However, check the manufacturer’s guidelines for your specific pump model.
Are all insulin pumps waterproof?
No, not all insulin pumps are waterproof. Some are water-resistant, meaning they can handle splashes or brief immersion, while others are entirely waterproof up to a certain depth and time limit. It’s crucial to know the difference and understand the limitations of your specific device.
What are some waterproof insulin pumps?
If you’re unsure which insulin pumps are waterproof, the ones listed below are at least confirmed water-resistant.
- Tandem T-slim X2 pumps: 1 m (3 ft) depth for up to 30 minutes (IP27).
- Dana Diabecare R: 1.5 m (5 ft) depth for up to 30 minutes (IPX-8).
- Omnipod 5: 7.6 m (25 ft) for up to 60 minutes (IP28).
- Medtronic MiniMed series: 3.6 m (12 ft) for up to 24 hours (IPX-8).
- Lifescan Animas Vibe : 3.6 m (12 ft) depth for up to 24 hours (IPX-8).
- Accu-Chek Spirit Combo : 2.4 m (8 ft) depth for up to 1 hour (IPX-8).
What should I do with my insulin pump when going for a swim?
If your insulin pump is not waterproof, you should disconnect and store it in a cool, dry place. If it is waterproof or water-resistant, ensure that all seals, caps, or covers are tightly closed before submersion. After swimming, inspect your pump for any water damage, and check the infusion site to ensure it remains secure.
How does chlorine or salt water affect the insulin pump?
Both chlorine and salt can be corrosive over time. While short exposure might not cause immediate damage, repeated and prolonged exposure can affect the pump’s casing, seals, and tubing. It’s recommended to rinse the pump with fresh water and dry it after swimming in chlorinated or salt water.
Can I use a waterproof case for my insulin pump while swimming?
Yes, there are waterproof cases designed for insulin pumps. These cases offer an added layer of protection, especially for pumps that aren’t inherently waterproof. Always ensure the case is securely closed and check its integrity regularly for signs of wear or damage.
What happens if my insulin pump gets wet?
If your insulin pump gets wet and it’s not designed to be waterproof, turn it off and remove the battery (if possible). Dry it thoroughly with a soft cloth. Avoid using heat or direct sunlight. Check the manufacturer’s guidelines on how to handle water exposure and contact their customer service if needed.
Is the adhesive for the infusion set water-resistant?
Most infusion sets are designed with adhesives meant to withstand sweat and minor water exposure. However, prolonged immersion might weaken the adhesive. After swimming, always check to ensure the infusion set remains secure and hasn’t become loose or detached.
Will extreme water temperatures impact the functionality of my pump or the insulin inside?
Yes, extreme temperatures can affect both the pump and the insulin. Cold water can make insulin less effective, and hot water can break it down faster, making it less potent. The pump’s electronics and battery can also be affected by temperature extremes. It’s advisable to avoid hot tubs and very cold water when wearing the pump.
How should I manage my blood sugar levels during and after swimming?
Swimming is a physical activity that can lower blood sugar levels. Before swimming, check your blood sugar. If it’s low, eat a snack. Monitor your levels after swimming as well. If you disconnect your pump for swimming, keep track of the time you’re off the pump and consider a bolus dose of insulin if you’ll be disconnected for an extended period.
How long after swimming should I wait before reconnecting my pump if I’ve disconnected it?
If you’ve disconnected your pump for swimming, you can typically reconnect it once you’ve dried off, and the infusion site is clean and dry. Always check your blood sugar levels when reconnecting and monitor them closely for a few hours afterward.
Does water activity affect insulin absorption or sensitivity?
Yes, physical activities, including swimming, can increase insulin sensitivity. This means that your body might use insulin more effectively, and you may experience a more significant drop in blood sugar levels. Always monitor your blood sugar before, during, and after swimming to ensure you remain within a safe range.
Is there a risk of infection if the infusion site remains wet for extended periods?
Yes, keeping the infusion site wet for prolonged periods can increase the risk of bacterial growth and potential infection. After swimming or any prolonged water exposure, ensure the site is clean and dry. If you notice any signs of infection, like redness, swelling, or discharge, consult your healthcare provider.
How do you cover the insulin pump site while swimming?
Here are some methods and products that can be used to cover the insulin pump site while swimming:
- Waterproof Dressings or Patches: These are adhesive patches designed to be worn over the infusion set. They provide a waterproof barrier, helping to keep the site dry and secure. Popular brands include Tegaderm and Opsite Flexifix.
- Silicone Covers: These are reusable and flexible covers that can be placed over the infusion set. They form a seal around the site to prevent water from entering. Products like the Skin Grip or StayPut Medical patches are designed for this purpose.
- Waterproof Tapes: Medical-grade waterproof tapes can be used to secure the edges of the infusion set, providing extra adhesion and water protection. Hypafix or 3M’s Transpore are examples.
- Swim Caps for the Body: Think of these as large swim caps but designed for body parts. You can use them to cover larger areas, such as the abdomen or thigh, where the infusion set might be located. They are made of waterproof materials and provide a tight seal.
- Waterproof Cases or Pouches: If you’re wearing your insulin pump while swimming, you can use waterproof pouches or cases designed for pumps. They can be worn around the waist or other parts of the body, keeping the pump dry while swimming.
- DIY Solutions: Some individuals use everyday items like plastic wrap combined with waterproof tape to create a temporary water barrier over the infusion site. While not as reliable as medical-grade solutions, they can work in a pinch.
- Specialized Swimwear: Some companies produce swimwear with integrated pockets or pouches designed to hold and protect medical devices like insulin pumps.
When considering any of these solutions, always:
- Test before prolonged use: Before diving in or swimming for an extended period, test your chosen method to ensure it’s watertight and adheres well to your skin.
- Inspect after swimming: After swimming, always check the infusion site for any signs of water infiltration, irritation, or adhesive failure.
- Change as needed: If you notice that the infusion set adhesive has weakened or that the site seems compromised after swimming, consider changing the set.
What precautions should I take with my Continuous Glucose Monitor (CGM) while swimming?
If your Continuous Glucose Monitor (CGM) is integrated with your insulin pump, swimming brings in a set of considerations to ensure both accurate glucose readings and the safety of your devices. Here are some precautions to take:
- Check the Waterproof Ratings: Just like with insulin pumps, not all CGMs are waterproof. Before swimming, check the manufacturer’s guidelines for your specific CGM model to determine its water resistance or waterproof capabilities.
- Secure the Sensor: The CGM sensor is attached to your body with an adhesive. Water and physical activity can weaken this adhesive. Consider reinforcing the adhesive with medical-grade tape, a waterproof patch, or specialized adhesive products designed for CGMs.
- Avoid Direct Impact: High dives, water slides, or other high-impact water activities can dislodge or damage the sensor. It’s best to be cautious and mindful of the sensor’s location during such activities.
- Rinse After Swimming: Chlorine from pools and salt from the ocean can leave residues that can potentially interfere with the adhesive or irritate the skin. Rinse off with fresh water after swimming and pat the area around the sensor gently to dry.
- Monitor Your Readings: Water exposure can sometimes affect the readings from your CGM. After swimming, monitor your glucose levels more frequently to ensure the CGM is still providing accurate data. If you see erratic or implausible readings, calibrate your CGM with a fingerstick measurement.
- Check Connectivity: Ensure that your CGM is still communicating with your pump after you’ve finished swimming. Sometimes, water can interfere with the wireless connection.
Additional Sources:
- https://www.canr.msu.edu/news/swimming_while_wearing_an_insulin_pump
- https://www.diabetes.co.uk/insulin-pumps/swimming-and-insulin-pumps.html
Photo Credit: VCU Capital News Service (CC BY-NC 2.0)

